
Hysteroscopy is a procedure that allows inspection of the uterus by using a telescope-like instrument called a hysteroscope.
Hysteroscopy is a procedure that allows a physician to look through the vagina and neck of the uterus (cervix) to inspect the cavity of the uterus. A telescope-like instrument called a hysteroscope is used. Hysteroscopy is used as both a diagnostic and a treatment tool.
Diagnostic hysteroscopy may be used to evaluate the cause of infertility, to determine the cause of repeated miscarriages, or to help locate polyps and fibroids.
The procedure is also used to treat gynecological conditions, often instead of or in addition to dilatation and curettage (D&C). A D&C is a procedure for scraping the lining of the uterus. A D&C can be used to take a sample of the lining of the uterus for analysis. Hysteroscopy is an advance over D&C because the doctor can take tissue samples of specific areas or actually see fibroids, polyps, or structural abnormalities.
When used for treatment, the hysteroscope is used with other devices to remove polyps, fibroids, or IUDs that have become embedded in the wall of the uterus.
Diagnostic hysteroscopy is performed in either a doctor's office or hospital. Before inserting the hysteroscope, the doctor injects a local anesthetic around the cervix. Once it has taken effect, the doctor dilates the cervix and then inserts a narrow lighted tube (the hysteroscope) through the cervix to reveal the inside of the uterus. Ordinarily, the walls of the uterus are touching each other. In order to get a better view, the uterus is inflated with carbon dioxide gas or fluid. Hysteroscopy takes about a half hour,Treatment involving the use of hysteroscopy is usually performed as a day surgical procedure with regional or general anesthesia. Tiny surgical instruments are inserted through the hysteroscope, and are used to remove polyps or fibroids. A small sample of tissue lining the uterus is often removed for examination, especially if there is any abnormal bleeding.
If the procedure is done in the doctor's office, the patient will be given a mild pain reliever before the procedure to ease cramping. The doctor will wash the vagina and cervix with an antiseptic solution.
If the procedure is done in the hospital under general anesthesia, the patient should not eat or drink anything (not even water) after midnight the night before the procedure.
Many women experience light bleeding for several days after surgical hysteroscopy. Mild cramping or pain is common after operative hysteroscopy, but usually fades away within eight hours. If carbon dioxide gas was used, there may also be some shoulder pain. Nonprescription pain relievers may help ease discomfort. Women may want to take the day off and relax after having hysteroscopy.
Diagnostic hysteroscopy is a fairly safe procedure that only rarely causes complications. The primary risk is prolonged bleeding or infection, usually following surgical hysteroscopy to remove a growth.
Very rare complications include perforation of the uterus, bowel, or bladder. Surgery under general anesthesia causes the additional risks typically associated with anesthesia.
Patients should alert their health care provider if they develop any of these symptoms:
A normal, healthy uterus with no fibroids or other growths.
Using hysteroscopy, the doctor may find uterine fibroids or polyps (often the cause of abnormal bleeding) or a septum (extra fold of tissue down the center of the uterus) that can cause infertility. Sometimes, precancerous or malignant growths are discovered.
A benign tumor of the uterus
A growth that projects from the lining of the cervix, the nose, or any other mucus membrane.
A condition present at birth in which there is an extra fold of tissue down the center of the uterus that can cause infertility. This tissue can be removed with a wire electrode and a hysteroscope.
Submucous fibroids can usually be treated by hysteroscopic resection provided they are less than 10 cm in diameter. Usually a gonadotrophin releasing hormone analogue GnRH-a (as used for pituitary suppression in IVF programmes) will be given by either nasal inhalation, or subcutaneous injection either daily or monthly for between two and eight weeks prior to surgery. This will cause low levels of oestrogen and may cause some shrinkage of the fibroid together with thinning of the endometrium, which will make the operation easier.
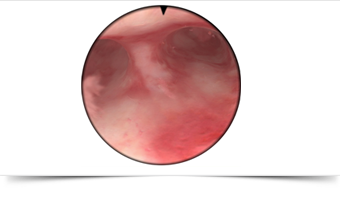
The fibroid is resected using a wire loop passed down an operating hysteroscope, an instrument of up to 9mm in diameter which is introduced into the uterus via the cervix after it has been gently dilated (stretched) to allow the hysteroscope to pass. A new diathermy instrument called a Versapoint and some lasers can be used in a similar fashion, to either cut through the base of the fibroid or, at higher power settings, they can completely vaporise smaller fibroids.
Hysteroscopic procedures are quite straightforward provided the surgeon has had proper training, but there are some complications of which you should be aware. As with any other operation, there is a risk of infection and bleeding. There is also a risk that the instrument may perforate the uterus and damage the bowel or blood vessels of the pelvis with potentially catastrophic results. Thankfully these complications are now very rare, since thorough training programmes have been introduced. The other problem with hysteroscopic procedures is the absorption of the distension medium (fluid which is used to distend the cavity of the uterus to ensure a good view) through small blood vessels which are inevitably cut during the operative procedure. This absorption can cause disturbance of the sensitive salt and water balance of the body causing headaches, nausea and in some cases swelling of the brain. These effects are usually minor provided no more than 1 litre of fluid enters the circulation. In some cases, particularly with large fibroids the resection may have to be completed in two stages due to excessive fluid absorption.
The surgical removal of fibroids is called a myomectomy. Intramural and subserous fibroids up to 10 cm in diameter can be removed by laparoscopic myomectomy, through two small incisions 10 mm in length, one in the umbilicus (navel) and the other a little lower down in the midline of the abdomen. Two smaller incisions only 5mm in length are made, one on either side of the abdomen about three inches from the midline. Presently only a handful of surgeons in this country offer this procedure which takes much longer and is more challenging than conventional surgery. The picture below, on the left, is of an intramural fibroid of 5 cm in diameter prior to removal laparoscopically. The picture on the right shows the appearance after removal and laparoscopic repair.
The principal difficulty with laparoscopic myomectomy is the repair of the uterus after the fibroid has been removed. This is done using laparoscopically applied sutures which requires considerable experience, training and a great deal of patience. After removal of the fibroid, it has to cut into thin strips of 10mm in diameter so that it can be removed, piecemeal through one of the laparoscopic ports. This is done with an instrument called a morcellator, seen in the foreground of the picture below. It consists of two concentric cylinders, the inner one has a sharp blade at the end and is driven to rotate by an electric motor.
Results for laparoscopic surgery performed in the best centres are comparable with conventional surgery. The advantages as far as the woman is concerned are a shorter spell in hospital, less post-operative pain and a faster return to work. However, not all fibroids are suitable for laparoscopic management and some may require conventional surgery, especially if there are three or more discreet fibroids present, or the fibroid is positioned such that access is restricted.
Enter your details below & we will call you back